Q: Why are deaths not as high as in the Spring?
A: There is no evidence that the virus itself has become milder.
The lower numbers of deaths we see now compared to equivalent numbers of cases in the Spring is likely due to 3 main factors:
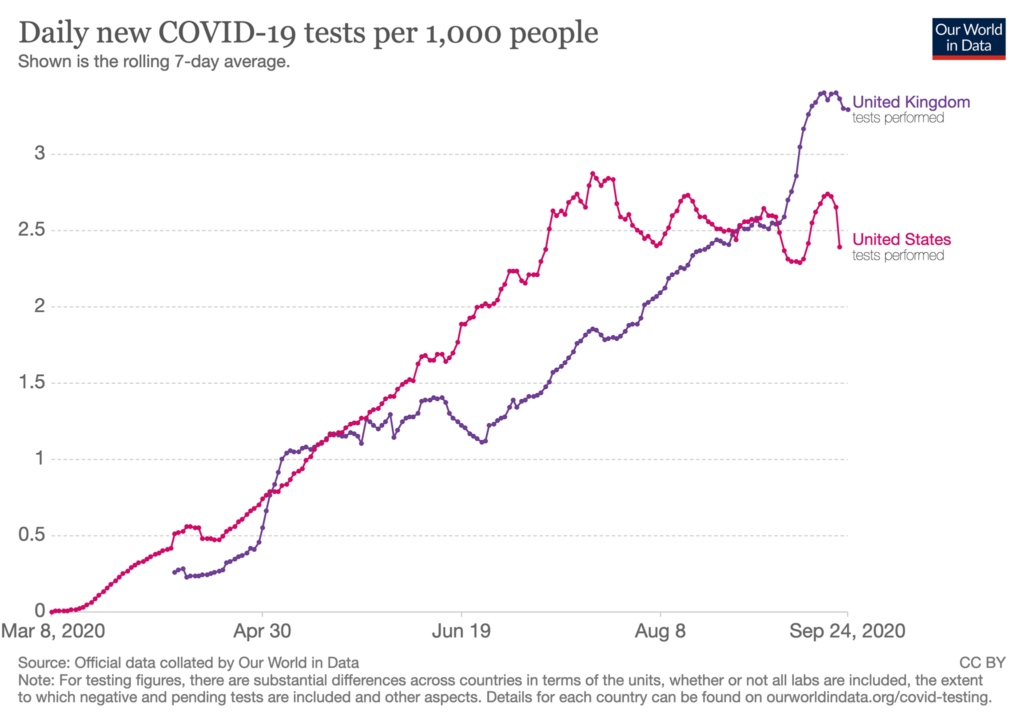
1) MORE TESTING: Early in the pandemic we were measuring the tip of the iceberg of cases, picking up only the most severe cases.
2) CHANGES IN AGES OF INFECTED: Younger people make up a larger fraction of new infections, as older and more vulnerable people continue to take more precautions even as lockdown measures ease.
3) IMPROVED TREATMENT FOR SICKEST PATIENTS: Clinicians have improved treatment protocols for severely ill patients, reducing mortality among those hospitalized. While good news, this effect is not believed to be large, however.
As we pass the sober milestone of 200,000 confirmed U.S. COVID-19 deaths and almost 1,000,000 globally, we would all welcome good news about COVID-19 getting less severe.
While the U.S. case fatality rate (CFR), or % dying among confirmed cases, has fallen from over 6% to around 3% (see figure) this is still a frighteningly high number, amounting to close to 700 new US COVID deaths a day. The CFR is also very sensitive to the amount of testing.
The infection fatality rate (IFR) is the % dying among *all* infections, even those we don’t confirm with testing. This is the number we *really* want to know as it tells us the true lethality of the disease.
The challenge with the IFR is we need to estimate how many people have actually been infected. We typically do this with seroprevalence studies, where we test blood samples for antibodies that indicate previous exposure to SARS-CoV-2, and calculate the % of the population has been infected.
In this piece in STAT news, Dr. Douglas Rothman takes seroprevalence estimates from Arizona (12.9%) from July and calculates an overall IFR of 0.63%, comparable to equivalent estimates in the Spring. He also finds no evidence that the ratio of deaths per hospitalization has been different in Arizona compared to New York City which had an earlier outbreak. This argues against the virus getting less deadly and in favor of changes in testing and the age distribution of cases.
Improved care is heartening; clinicians are better at assessing the need for and timing of interventions such as mechanical ventilation as well as benefiting from treatments including dexamethasone. Hospital capacity is not as overwhelmed as it was in the Spring.
What about virus mutation? While it’s true that the D614G variant of the coronavirus has become much more prevalent over time, possibly due to luck, so far the evidence does not support this variant being less deadly, with a recent study finding no difference in risk of death in patients who had one variant versus the other.
BOTTOM LINE: Nothing fundamental has changed about the virus, and it remains a deadly threat. Our efforts to protect the most vulnerable compared to the Spring are surely helping, along with improved critical care.
Given that the we don’t live in age or risk segregated bubbles, we must remain vigilant to keep transmission low and minimize avoidable deaths while vaccines & new treatments remain on the horizon.
We mourn each and every one of the 1,000,000 global COVID-19 deaths thus far, and remind readers that these are very likely UNDERESTIMATES of deaths (see previous DP post on excess mortality.).
Thanks to followers Devin and Barb from Illinois for this excellent question from the question box (found at the bottom of our website, www.dearpandemic.org).
#StaySMART, stay safe and stay sane.
Love,
Those Nerdy Girls
Additional Links:
Changing Age Distribution of the COVID-19 Pandemic in the U.S.