A: The answer depends on age, breast cancer risk, and more.
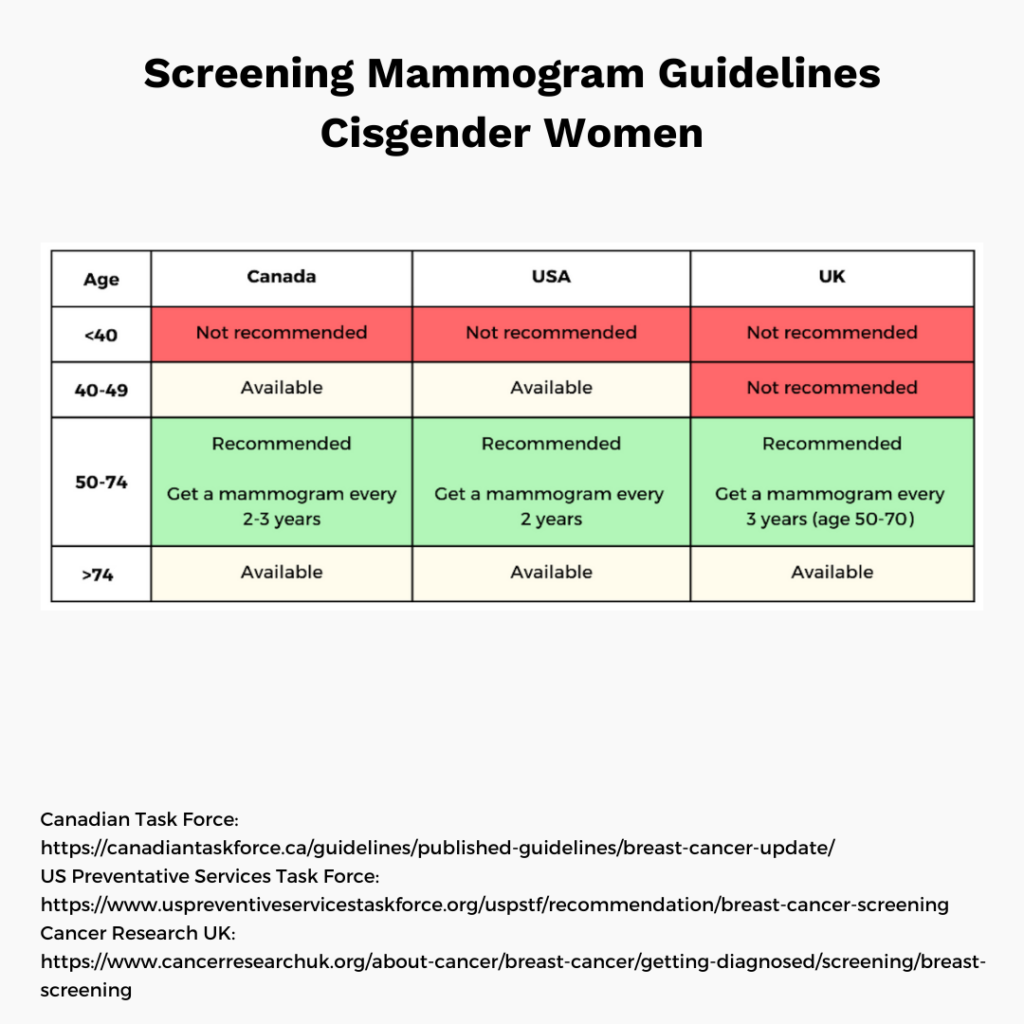
For average risk cisgender women, regular screening mammograms are widely recommended from age 50 to 70. Earlier and later in life, the balance of benefits and risks is murkier in this population. There are additional considerations for those at higher risk of cancer, and for nonbinary and transgender people.
Screening mammography is a powerful tool that can save lives, but it’s far from perfect. Let’s take a closer look at the potential benefits and risks, and how the balance varies across populations.
BENEFITS
✅ Screening mammography helps catch tumors that are smaller and easier to treat, with better outcomes.
➡ A recent study for the US Preventive Services Task Force (USPSTF) looked at average-risk women screened with mammography over 10 years. Over 10 years, mammography saved roughly 8 lives per 10,000 people (ages 50-59), 21 lives per 10,000 people (ages 60-69) and 13 lives per 10,000 people (ages 70-74). For ages 39-49 the benefits were unclear (not statistically significant).
✅ Mammograms can offer peace of mind, as most will come back normal.
RISKS
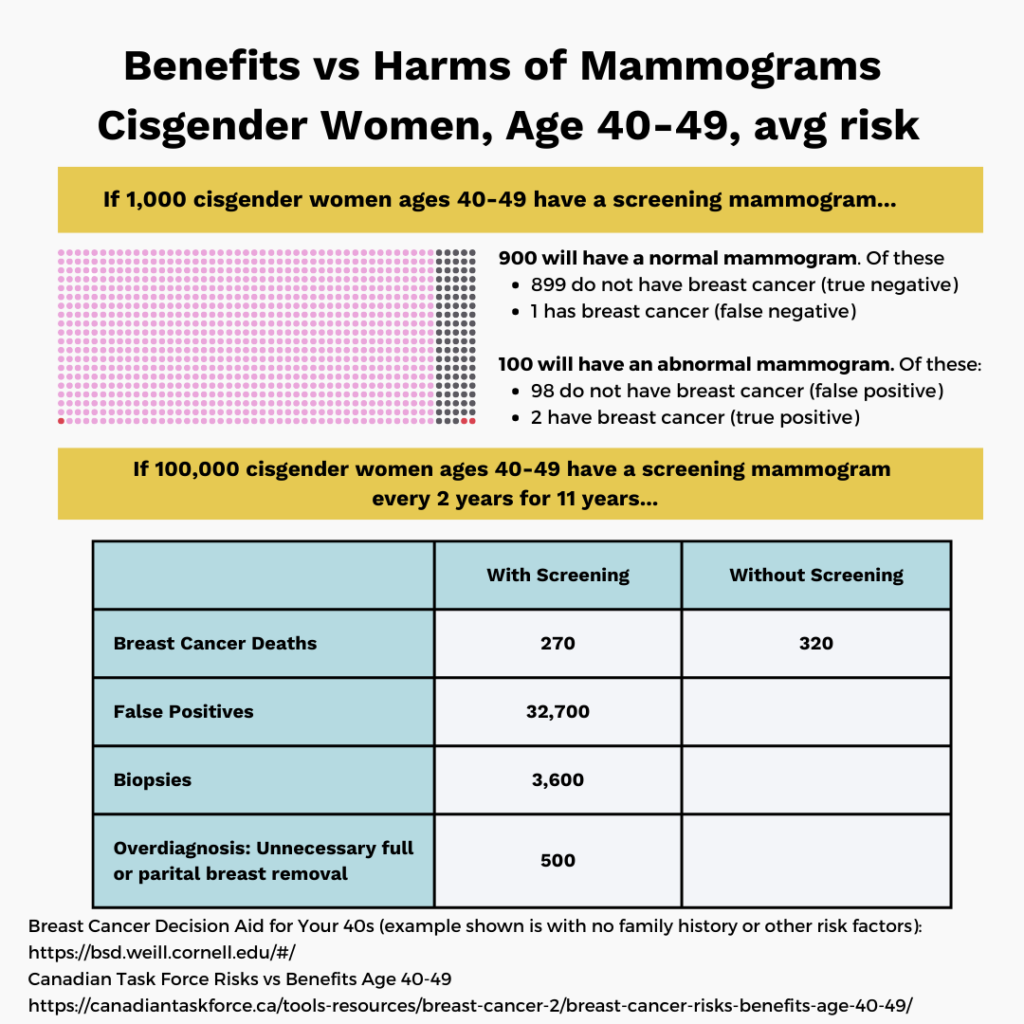
❌ False positives: Abnormal mammograms are sent for follow up testing (imaging or biopsy and often turn out to be false alarms. This can be a major burden physically, psychologically, and financially.
➡ Roughly half of average risk women in the United States will experience a false positive over 10 years of screening (per USPSTF study).
❌ Overdiagnosis: Overdiagnosis is defined as treating tumors that would never have caused major health issues or death. We know that overdiagnosis is a real issue with breast cancer screening because the mortality benefits (lives saved) are modest compared to the major increase in cancer surgeries and therapies. Part of the issue is that slow-growing tumors are easier to catch by mammogram than rapidly-growing ones. Unfortunately, doctors can’t always predict which tumors can safely be left untreated.
➡ Roughly 11 to 22 percent of cases may be overdiagnosed (unnecessary treatments), according to the recent USPSTF study. This issue affects all age groups.
❌ Underdiagnosis (false negatives): Mammograms don’t catch every tumour during the critical early stages. Dense breast tissue can increase the risk of underdiagnosis.
➡ Regular screening reduces the risk of dying from breast cancer by about 25-30% in average risk women, according to the USPSTF study.
❌ Radiation: With frequent screening, small doses of radiation can add up over time.
SCREENING GUIDELINES
The balance of benefits to risks depends on who is being screened. It tends to be more favourable in higher risk people, either due to age or other factors.
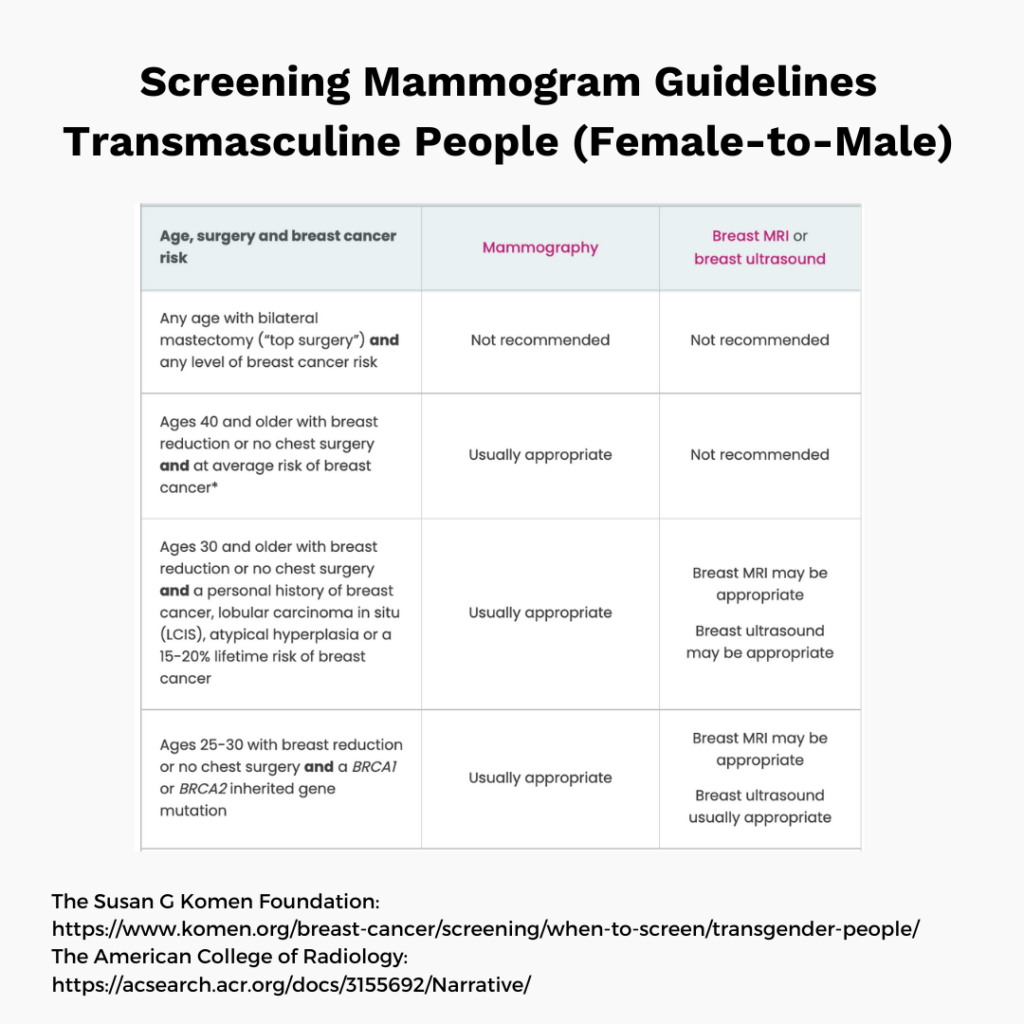
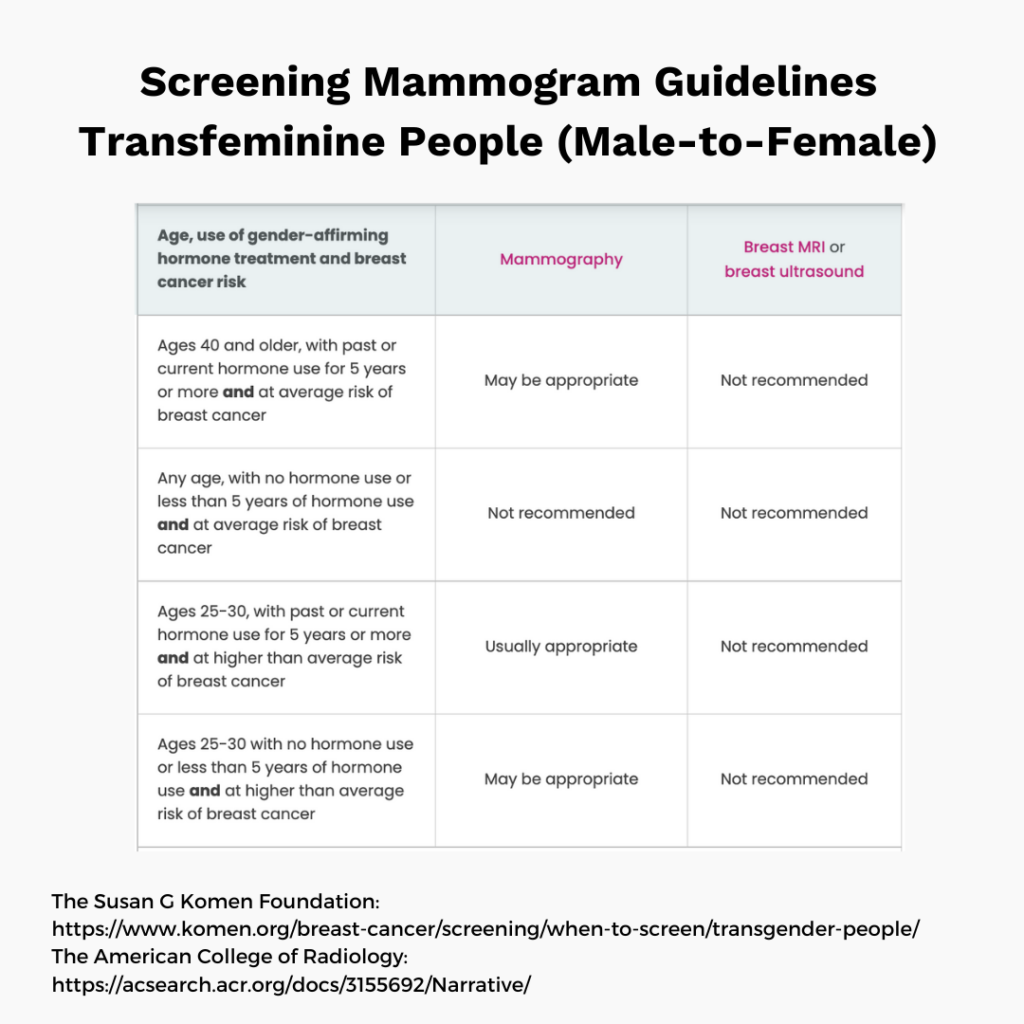
Regular screening mammograms are widely recommended for average risk cisgender women for ages 50-70 and for certain transgender or non-binary people. Routine mammography is not recommended for cisgender men of average risk.
Before age 50 and after age 70, guidelines vary regionally, and personal considerations are vital – things like how you feel about the possibility of false positives or overdiagnosis.
❗Higher-risk individuals should discuss the benefits and risks of screening with their healthcare practitioner. Earlier or more frequent screening may be advised.
NB: Average risk for cisgender women is defined as: No personal history of breast cancer. No history of breast cancer in a first-degree relative. No known mutations in BRCA1/2 genes. No previous exposure of the chest wall to radiation
👉 See below for screening guidelines (average risk cisgender women and transgender people) and a closer look at benefits vs risk for ages 40-49.
OUR TAKE
Those Nerdy Girls get (or plan to get) screening mammograms from age 50-74 as advised by the USPSTF and Canadian Task Force. We have made different choices about the optimal time to start screening. Some began at age 40 or earlier (based on risk factors and personal choice), some waited until age 50, and others landed in between.
👉 To make your screening plan, consult national guidelines, talk to your doctor about your risks factors, and educate yourself about what to expect. Also, try the online tool below.
WHAT TO EXPECT
Ready to take the plunge? During mammography, a technician presses your breast between two plates then takes an x-ray image. It can be mildly uncomfortable through painful (but brief). Next, you wait for the results. If things look normal, you’re in the clear until your next exam. If not, you’ll be sent for follow-up tests – this can include imaging and/or biopsy. As discussed, we often find that there is nothing to worry about.
Stay safe. Stay well.
Those Nerdy Girls
Additional LinksBreast screening decision tool for your 40s (Weill Cornell)